
Arthritis and rheumatoid arthritis are among the most common chronic joint diseases affecting people across all ages, especially adults over 40. These conditions can cause pain, stiffness, swelling, and limited movement that may severely impact daily life. Understanding their causes, symptoms, and treatments is essential for effective management and improved quality of life.

In this comprehensive review, we’ll explore everything about arthritis and rheumatoid arthritis (RA disease): what they are, their causes, signs and symptoms, available treatments, and modern medical and natural approaches to relief. We’ll also include expert guidance from top health organizations such as the Arthritis Foundation, Mayo Clinic, and NCBI.
What Is Arthritis and Rheumatoid Arthritis?
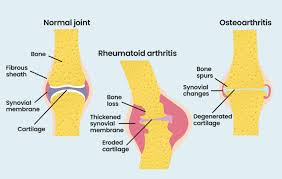
The term arthritis refers to inflammation of one or more joints. It is not a single disease but a general term encompassing more than 100 related conditions. The two most common forms are osteoarthritis (OA) and rheumatoid arthritis (RA).
While osteoarthritis typically develops due to wear and tear on joints over time, rheumatoid arthritis is an autoimmune disorder — meaning the body’s immune system mistakenly attacks its own tissues, particularly the synovium (the lining of the membranes surrounding the joints).
Rheumatoid Arthritis (RA) Definition
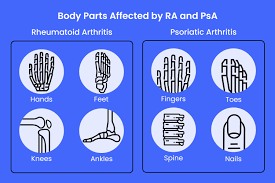
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that affects the joints symmetrically — usually the wrists, hands, knees, and ankles. Over time, it can lead to bone erosion, joint deformity, and systemic complications involving the skin, eyes, lungs, heart, and blood vessels.
Unlike other types of arthritis, RA disease is systemic and progressive, requiring early diagnosis and continuous management under the supervision of a rheumatologist.
Causes of Arthritis and Rheumatoid Arthritis
The causes of arthritis vary depending on the specific type. Common causes include:
- Genetics – A family history of arthritis increases risk.
- Age – Risk increases with age as cartilage naturally wears down.
- Gender – Women are more likely to develop rheumatoid arthritis.
- Injury – Joint injuries can trigger arthritis later in life.
- Obesity – Excess weight puts pressure on joints, especially the knees, hips, and spine.
- Infections – Certain viral or bacterial infections can trigger joint inflammation.
- Immune system dysfunction – In rheumatoid arthritis, the immune system attacks healthy joint tissue.
Specific Causes of Rheumatoid Arthritis
While the exact cause of RA is still unclear, research suggests a combination of genetic, environmental, and hormonal factors may contribute.
Some potential triggers include:
- Abnormal immune response to bacteria or viruses
- Smoking – a major risk factor for developing RA and worsening symptoms
- Hormonal imbalances, particularly in women
- Epigenetic changes affecting immune system regulation
For more scientific insight, visit the National Center for Biotechnology Information (NCBI).
Signs and Symptoms of Rheumatoid Arthritis
Recognizing the early rheumatoid arthritis symptoms is crucial for timely intervention. Common symptoms include:
- Joint pain and stiffness, especially in the morning
- Swelling and warmth around affected joints
- Fatigue and weakness
- Loss of appetite
- Low-grade fever
- Symmetrical joint involvement (both sides of the body)
- Joint deformities over time if untreated
Other systemic symptoms can include dry eyes, shortness of breath, or nodules under the skin.
If you experience these signs, consult a rheumatologist for proper diagnosis and testing.
How Rheumatoid Arthritis Is Diagnosed
A rheumatologist uses several approaches to confirm RA disease diagnosis, including:
1. Physical Examination
The doctor checks for joint tenderness, swelling, redness, and warmth. They may assess your range of motion and overall joint function.
2. Blood Tests
Blood tests help identify markers of inflammation and immune activity:
- Rheumatoid factor (RF)
- Anti-CCP antibodies
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
3. Imaging Tests
- X-rays – to check for joint damage
- MRI and Ultrasound – to detect early inflammation and erosion
Early diagnosis allows better management and reduces the risk of permanent joint damage.
Treatment Options for Arthritis and Rheumatoid Arthritis
While there is no definitive cure, treatments aim to reduce inflammation, relieve pain, and prevent further joint damage. The treatment plan usually combines medication, therapy, and lifestyle changes.
1. Medications for Rheumatoid Arthritis
A rheumatologist typically prescribes medications based on the disease’s severity and progression.
a. NSAIDs (Nonsteroidal Anti-Inflammatory Drugs)
These drugs help relieve pain and reduce inflammation.
Examples: ibuprofen, naproxen.
b. Corticosteroids
Powerful anti-inflammatory drugs such as prednisone are used for flare-ups but should be limited to short-term use due to side effects.
c. DMARDs (Disease-Modifying Antirheumatic Drugs)
These medications slow the progression of RA disease and prevent joint damage.
Common DMARDs: methotrexate, sulfasalazine, leflunomide.
d. Biologic Agents
Biologic DMARDs target specific components of the immune system to control inflammation.
Examples: adalimumab, etanercept, infliximab.
e. JAK Inhibitors
A newer class of medication that blocks inflammatory pathways.
Examples: tofacitinib, baricitinib.
2. Physical Therapy and Exercise
Physical therapy helps maintain flexibility and strengthen muscles around affected joints.
Recommended exercises include:
- Gentle stretching
- Swimming
- Walking
- Yoga and tai chi
Always consult your doctor before starting any exercise program.
3. Lifestyle Modifications
Making lifestyle changes is key to managing arthritis and rheumatoid arthritis effectively:
- Maintain a healthy weight to reduce joint stress
- Stop smoking – it worsens RA symptoms
- Eat an anti-inflammatory diet (rich in omega-3, fruits, and vegetables)
- Manage stress with relaxation techniques
- Get enough sleep for immune recovery
4. Surgical Treatments
When joint damage becomes severe and non-surgical treatments fail, surgery might be recommended:
- Synovectomy (removal of inflamed synovium)
- Tendon repair
- Joint fusion
- Total joint replacement (hip or knee)
Get Your Ultimate Guide to Rheumatoid Arthritis Now!
Are you struggling with rheumatoid arthritis or worried about the early signs of RA? Don’t wait until the pain gets worse! Our comprehensive eBook, Rheumatoid Arthritis: Causes, Solutions, Treatments & Prevention, is your complete guide to understanding RA, managing symptoms, and preventing joint damage.
Inside this eBook, you’ll discover:
- Detailed explanations of rheumatoid arthritis symptoms and RA symptoms
- Proven strategies for rheumatoid arthritis treatment
- How to recognize early signs of rheumatoid arthritis before serious damage occurs
- Lifestyle tips, exercises, and diet plans for arthritis in fingers and other affected joints
- Expert advice for living a healthy, active life with RA
Don’t let rheumatoid arthritis control your life! Take the first step towards relief and empowerment.
Click here to get your eBook now!
Why you need this eBook:
- Easy-to-understand language, perfect for anyone dealing with RA
- Actionable solutions and preventive measures you can implement today
- Professional, science-backed guidance from experts in autoimmune health
Take control of your health—get your copy today and start managing your RA like a pro!
Natural and Complementary Therapies for Arthritis and Rheumatoid Arthritis
In addition to medical treatments, some people find relief through natural remedies and alternative therapies:
- Fish oil supplements (omega-3 fatty acids reduce inflammation)
- Turmeric (curcumin) – a natural anti-inflammatory spice
- Acupuncture – may help relieve pain and stiffness
- Massage therapy – improves circulation and joint mobility
- Heat and cold therapy – reduce swelling and pain
Always consult your doctor before starting alternative treatments.
The Role of a Rheumatologist in Managing RA Disease
A rheumatologist is a specialist trained to diagnose and treat arthritis and autoimmune diseases. Regular visits to a rheumatologist help:
- Monitor disease activity
- Adjust medications as needed
- Prevent complications
- Educate patients on self-management
For accurate information on rheumatoid arthritis care.
Living with Arthritis and Rheumatoid Arthritis
Living with RA can be challenging, but many patients manage symptoms successfully through proper care.
Here are some daily management tips:
- Keep a joint-friendly routine with gentle exercises
- Use assistive devices (like braces or ergonomic tools)
- Prioritize mental health and support groups
- Keep a symptom diary to track flares and triggers
- Stay consistent with medication and check-ups
Diet and Nutrition for Rheumatoid Arthritis
A balanced, anti-inflammatory diet plays a key role in managing symptoms.
Foods to Eat
- Fatty fish (salmon, mackerel, sardines)
- Olive oil
- Nuts and seeds
- Leafy greens
- Berries
Foods to Avoid
- Processed foods
- Red meats
- Sugary beverages
- Refined carbohydrates
Proper nutrition supports the immune system and reduces inflammation in RA disease.
Boost Your Joint Health with JointVive
A Unique Solution for Comfort, Flexibility, and Mobility
For those looking for extra support in managing joint discomfort and maintaining mobility, JointVive can be a game-changer. Unlike anything else on the market, JointVive is crafted from a unique blend of rare, hard-to-source ingredients designed to help support joint comfort, flexibility, and overall mobility. Combined with proper lifestyle habits and RA management strategies, JointVive may provide the additional boost your joints need to stay active and pain-free. Don’t wait—take control of your joint health today! Click here to get JointVive now and start feeling the difference.
Early detection in fingers allows for prompt treatment and prevents permanent deformities.
Natural Remedies for Arthritis and Rheumatoid Arthritis
Emotional and Psychological Impact
RA doesn’t just affect the body — it also impacts emotional well-being. Chronic pain can lead to anxiety, depression, and fatigue. Support groups, therapy, and open communication with family are essential to maintaining mental balance.
Future of Rheumatoid Arthritis Treatments
Medical research continues to advance, aiming to improve outcomes for RA patients. Emerging areas include:
- Gene therapy to regulate immune response
- Stem cell therapy for cartilage regeneration
- Personalized medicine tailored to genetic profiles
For ongoing studies, refer to the Mayo Clinic research section.
How a Rheumatologist Treats Arthritis and Rheumatoid Arthritis
A rheumatologist is the primary specialist responsible for diagnosing and managing arthritis and rheumatoid arthritis. Their goal is to control inflammation, relieve pain, and prevent long-term joint damage. Treatment usually begins with a detailed evaluation, including blood tests and imaging, to identify the severity of joint inflammation. Based on this assessment, the rheumatologist develops a personalized plan that often includes DMARDs (disease-modifying antirheumatic drugs), biologic therapies, and anti-inflammatory medications. Regular follow-ups help track progress and adjust medications to achieve remission or minimal disease activity.
Beyond medication, a rheumatologist also focuses on patient education and lifestyle modification to improve overall joint health. Patients with arthritis and rheumatoid arthritis are encouraged to maintain a healthy diet, engage in low-impact exercise, and stop smoking to reduce flare-ups. In some cases, physical therapy and occupational therapy are recommended to strengthen muscles and protect joint function. By combining medical treatment with lifestyle support, rheumatologists help patients live fuller, more comfortable lives despite chronic joint disease.
FAQ – Frequently Asked Questions about Arthritis and Rheumatoid Arthritis
1. What is the difference between arthritis and rheumatoid arthritis?
Arthritis is a general term for joint inflammation, while rheumatoid arthritis is a specific autoimmune disease causing chronic joint damage.
2. What are the first signs of rheumatoid arthritis?
Early signs include joint stiffness in the morning, swelling, pain, fatigue, and symmetrical joint pain (both sides of the body).
3. How is rheumatoid arthritis treated?
Treatment involves medications (DMARDs, biologics), physical therapy, healthy lifestyle habits, and sometimes surgery.
4. Can rheumatoid arthritis be cured?
There is currently no cure, but early treatment can lead to remission and prevent severe damage.
5. When should I see a rheumatologist?
If you experience persistent joint pain, stiffness, or swelling lasting more than six weeks, consult a rheumatologist for evaluation.
Conclusion: Managing Arthritis and Rheumatoid Arthritis for a Better Life
Arthritis and rheumatoid arthritis are complex but manageable conditions. With early diagnosis, proper treatment, and lifestyle adjustments, most people can maintain mobility and a good quality of life. Regular follow-up with a rheumatologist, a healthy diet, and staying active are key strategies for controlling RA disease.
Living with arthritis doesn’t have to mean living with pain — knowledge, consistency, and care make all the difference.
SEE ALSO: Rheumatoid Arthritis Therapies: A Complete Review
Disclaimer: This article is for informational purposes only and does not replace the advice of a healthcare professional. Consult a doctor or nutritionist before starting any supplementation. Some links in the text are affiliate links, which means we may receive a commission if you make a purchase. This does not impact the price for you and helps us continue to bring you quality content.

Um comentário em “Arthritis and Rheumatoid Arthritis: Treatments and Conditions”
Comentários estão encerrado.