
Introduction
The rheumatoid factor (RF) is one of the most recognized markers in autoimmune medicine. Whether you’ve just received a positive RF test result or are trying to understand how it connects to rheumatoid arthritis, this guide breaks down everything you need to know in simple, human terms.
Understanding Rheumatoid Factor
Rheumatoid factor is an autoantibody—a protein produced by the immune system that mistakenly targets the body’s own tissues. It binds to other antibodies (specifically the IgG type), forming immune complexes that can trigger inflammation, especially in the joints.
While RF is most commonly associated with rheumatoid arthritis (RA), it can also appear in other autoimmune diseases or even in healthy people, especially older adults. A positive rheumatoid factor test doesn’t automatically mean you have RA—but it’s an important clue that doctors use alongside symptoms, imaging, and other blood tests like anti-CCP.
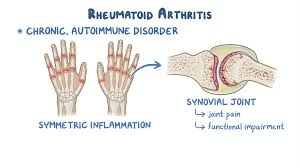
Rheumatoid Factor and Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune inflammatory arthritis that causes pain, swelling, and stiffness in multiple joints. RF is found in about 70–80% of RA patients, and when present in high amounts, it often indicates more active or severe disease.
People with high RF levels may experience:
- More rapid joint damage
- Increased inflammation markers (like ESR or CRP)
- Extra-articular symptoms such as fatigue, dry eyes, or lung inflammation
However, it’s possible to have seronegative RA—meaning you have all the symptoms of rheumatoid arthritis but no detectable RF in your blood.
Causes of Elevated Rheumatoid Factor
An elevated RF result can be caused by several conditions beyond rheumatoid arthritis. Some of the most common include:
- Autoimmune diseases such as Sjögren’s syndrome and lupus
- Chronic infections, including hepatitis C and tuberculosis
- Liver disease or chronic lung conditions
- Normal aging, where mild RF positivity can appear naturally
This is why context matters—a doctor must interpret RF results alongside your medical history, symptoms, and additional tests.
Diagnosis and Testing for Rheumatoid Factor
A rheumatoid factor test is a simple blood test that measures the amount of RF antibodies in your bloodstream.
Results are usually expressed in IU/mL (international units per milliliter).
- A negative result (<14 IU/mL) generally suggests the absence of RF.
- A positive result (≥14 IU/mL) may indicate rheumatoid arthritis or another inflammatory condition.
However, the test’s accuracy varies:
- Sensitivity for RA: around 70–80%
- Specificity: lower, since other diseases can raise RF levels
To confirm rheumatoid arthritis, doctors often order additional tests, including:
- Anti-CCP (anti-cyclic citrullinated peptide) antibodies — more specific for RA
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) for inflammation
- X-rays or MRI scans to detect joint erosion or inflammation
➡ External reference: Mayo Clinic – Rheumatoid Factor Test
Signs Rheumatoid Arthritis Is Getting Worse
If you already have rheumatoid arthritis and want to know whether your condition is worsening, pay attention to these signs:
- Increased joint stiffness lasting longer in the morning
- Swelling in new joints
- Persistent fatigue and weakness
- Subcutaneous rheumatoid nodules (small lumps under the skin)
- Difficulty performing daily tasks
- Noticeable deformities in fingers or wrists
High RF levels often correlate with more aggressive disease, but your doctor will consider multiple factors before adjusting treatment.
Unusual Symptoms of Rheumatoid Arthritis
While joint pain and stiffness are the most recognized symptoms, RA can affect other parts of your body—especially in RF-positive patients.
Some unusual or lesser-known symptoms include:
- Dry eyes and mouth (Sjögren’s overlap)
- Shortness of breath due to lung inflammation
- Skin rashes or vasculitis
- Nerve pain or tingling
- Unexplained low-grade fevers
- Weight loss or appetite changes
If you experience these symptoms, you should contact a rheumatoid arthritis doctor for an evaluation.
Treatment Options for Rheumatoid Factor–Positive Patients
There’s no single “cure” for rheumatoid arthritis, but modern medicine offers highly effective treatments that can slow progression, relieve pain, and improve quality of life.
Main Treatment Categories
- DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
- Methotrexate, sulfasalazine, leflunomide
- Reduce immune system overactivity and protect joints
- Biologic Therapies
- TNF inhibitors (adalimumab, etanercept)
- IL-6 blockers (tocilizumab)
- JAK inhibitors (tofacitinib, baricitinib)
- Corticosteroids & NSAIDs
- Used short-term to reduce inflammation and manage flares
Alternative and Natural Support
Some patients find additional relief through:
- Anti-inflammatory diets (rich in omega-3 and antioxidants)
- Physical therapy and gentle exercise
- Stress reduction techniques such as yoga or meditation
➡ External reference: Arthritis Foundation – Treatment Options
📘 Get Your Ultimate Guide to Rheumatoid Arthritis Now!
Are you struggling with rheumatoid arthritis or worried about the early signs of RA? Don’t wait until the pain gets worse! Our comprehensive eBook, Rheumatoid Arthritis: Causes, Solutions, Treatments & Prevention, is your complete guide to understanding RA, managing symptoms, and preventing joint damage.
👉 Click here to get your eBook now!
Why you need this eBook:
- Easy-to-understand language, perfect for anyone dealing with RA
- Actionable solutions and preventive measures you can implement today
- Professional, science-backed guidance from experts in autoimmune health
Self-Care Tips for Managing Rheumatoid Arthritis
Managing rheumatoid arthritis requires daily awareness and lifestyle adjustments. Here are simple, proven strategies:
1. Stay Active
Regular movement maintains flexibility and reduces stiffness. Try swimming, cycling, or walking—activities that don’t strain the joints.
2. Eat an Anti-Inflammatory Diet
Focus on:
- Fish, olive oil, nuts, and seeds
- Fresh vegetables and fruits
- Whole grains and lean proteins
3. Protect Your Joints
Avoid repetitive strain. Use supportive tools, ergonomic chairs, and take frequent breaks from typing or heavy lifting.
4. Manage Stress
Chronic stress can trigger inflammation. Practice mindfulness, meditation, or simple breathing exercises daily.
5. Work Closely with Your Doctor
Regular visits with your rheumatoid arthritis specialist help track disease progression and adjust treatment early.
➡ External reference: NCBI – Self-Management in Rheumatoid Arthritis
When to See a Rheumatoid Arthritis Doctor
You should see a rheumatologist if you experience:
- Joint pain lasting more than six weeks
- Swelling in multiple joints
- Morning stiffness
- Family history of autoimmune disease
- A positive rheumatoid factor test with symptoms
Early diagnosis can make a major difference in long-term outcomes and help prevent irreversible joint damage.
💪 Natural Support for Joint Comfort: Try JointVive
If you’re looking for a natural way to support joint comfort and flexibility, JointVive may be exactly what you need.
JointVive is unlike anything you’ve tried before — it’s based on a unique, closely guarded formula designed to help support joint comfort, flexibility, and mobility.
With its powerful blend of rare, high-quality ingredients, it helps your body naturally promote healthier joints, reduce discomfort, and support long-term mobility.
👉 Take the next step toward joint relief — try JointVive today and feel the difference.
FAQ – Rheumatoid Factor and Rheumatoid Arthritis
1. Can you have rheumatoid arthritis without rheumatoid factor?
Yes, it’s called seronegative rheumatoid arthritis, and it accounts for about 30% of cases. Other tests like anti-CCP help confirm the diagnosis.
2. What’s a normal range for rheumatoid factor?
Typically under 14 IU/mL, but each lab may vary slightly.
3. Can infections raise rheumatoid factor levels?
Yes. Conditions like hepatitis C or tuberculosis can temporarily raise RF levels.
4. Does a high RF mean I’ll have severe arthritis?
Not necessarily. High RF is linked with more aggressive disease on average, but lifestyle, treatment, and genetics also play roles.
5. Should I retest my RF over time?
Most doctors don’t rely on repeat RF testing to monitor progress; they look at symptoms and inflammation markers instead.
Conclusion
The rheumatoid factor is a powerful but imperfect tool. It helps doctors understand your immune system’s behavior and predict how rheumatoid arthritis might develop. A positive test doesn’t automatically mean you have the disease, but it does signal the need for further investigation and early care.
If you’ve tested positive for RF or have ongoing joint pain, talk to a rheumatoid arthritis doctor near you. Early treatment, lifestyle improvements, and knowledge are your best defense against long-term joint damage and discomfort.
SEE MORE:Rheumatoid Arthritis Symptoms
Disclaimer: This article is for informational purposes only and does not replace the advice of a healthcare professional. Consult a doctor or nutritionist before starting any supplementation. Some links in the text are affiliate links, which means we may receive a commission if you make a purchase. This does not impact the price for you and helps us continue to bring you quality content.

Um comentário em “Rheumatoid Factor: Causes, Testing, and Its Role in Rheumatoid Arthritis”